THE PROTOCOL PUT SIMPLY
We made it !
The protocol has been updated during the summer of 2020. The vast majority of the recommandations we formulated have been integrated in the new protocol !
You can read more about the update here.
This page is now archived and will not be updated in the future. It should be used only as a reference document regarding the first version of the protocol.
The Protocol put simply
The Protocol was developed in the context of the COVID-19 pandemic, in the event of a significant increase in the need for intensive care and insufficient resources to meet such a demand.
If there were insufficient beds, ventilators, or even human resources, it would be necessary to choose which patient would have access to intensive care.
The Protocol specifies the different criteria that should be used by health professionals to decide on a priority of service in the event of a shortage of resources.
The selection of these criteria was made on the basis of ethical principles, such as maximizing profits, proportionality and fairness.
Although the Protocol is not in effect at the moment, it could become so at any time if the pandemic situation worsens. It is currently widely distributed to healthcare professionals across the province, ready to be used if necessary.
You may consult the Protocol on the Quebec College of Physicians website.
However, the Quebec government has refused to release the exclusion criteria set out in Appendices B and C of the Protocol and therefore, they do not appear in the published document.
It will not be reserved solely for those patients with COVID-19.
The Protocol outlines three levels of triage, depending on demand and resources available. The higher the demand and the more limited the resources, the stricter the access criteria.
- Triage Step 1: Aims to exclude those with an 80% or higher risk of mortality
- Triage Step 2: Aim to exclude those with a 50% or higher risk of mortality
- Triage Step 3: Aim to exclude those with a 30% or higher risk of mortality
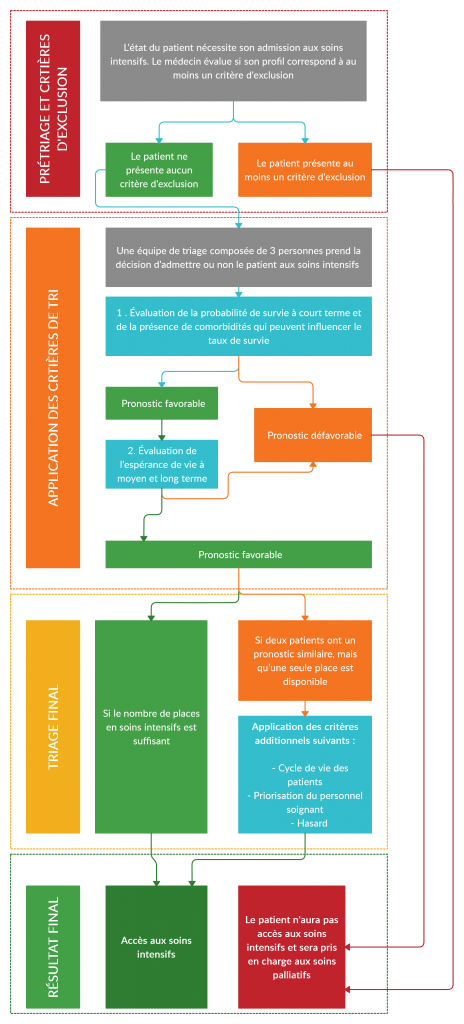
All patients are assessed first by the emergency physician to determine if they have one or more of the exclusion criteria.
If a patient presents at least one exclusion criterion, they cannot have access to intensive care. No assessment by a triage team is necessary.
If a patient presents no exclusion criteria, the doctor forwards an evaluation request to the triage team for further evaluation.
This triage team is made up of three people who come to a decision by consensus:
- An intensivist or emergency physician (president)
- A doctor from the establishment
- A non-doctor with appropriate clinical or management experience
The exclusion criteria provided for in the Protocol
The Protocol sets forth 12 exclusion criteria. A patient who meets at least one of these criteria is automatically ineligible for intensive care.
These criteria were selected because they indicate (according to the MSSS) a low probability of surviving an acute illness or a low probability of surviving more than a few months, regardless of the acute episode of the serious illness.
The exclusion criteria used are as follows:
- Trauma (TRISS score)
- Burn victims
- Cardiac arrest
- Severe cognitive impairment (total inability to perform activities of daily living and domestic life independently) due to progressive illness
- Advanced and irreversible neuromuscular disease (i.e., Parkinson’s, amyotrophic lateral sclerosis (ALS))
- Metastatic malignancy
- Severe and irreversible neurological event (i.e., intracerebral hemorrhage (ICH), WFNS classification, unfavorable ImPACT neurocognitive test results)
- Severe organ failure (i.e., Model for End-Stage Liver Disease (MELD))
- Functional capacity according to the Clinical Frailty Score (Geriatrics)
- Palliative surgery
- Extended mechanical ventilation
- Other clinical judgment
* In bold, those criteria posing ethical and legal dilemmas. For more information, see the related page.
Unfortunately, we have not yet been able to know the exclusion criteria used for pediatric patients. To date, the Government of Quebec has refused to share or disseminate this information.
If the number of patients awaiting intensive care exceeds the number of available beds, the following criteria are applied by the triage team to determine which patient will have access:
In order of importance:
- The probability of short-term survival and the presence of an associated condition which can influence the survival rate
- Medium- or long-term life expectancy
- The life cycle
- Priority for health care personnel
- Chance
People with disabilities and triage
The Protocol contains two exclusion criteria that may have an impact on people with intellectual disabilities:
- Severe cognitive impairment due to progressive disease
- Functional limitations assessed according to the Clinical Frailty Score
Remember that a patient presenting one or other of these criteria is automatically ineligible for intensive care, regardless of age and the reason for hospitalization.
Severe cognitive impairment due to progressive illness
A priori, a person with a cognitive impairment that is not linked to a progressive illness should not be refused access to intensive care based on this exclusion criterion. However, the mere presence of such a criterion in the Protocol leaves room for errors in application and interpretation by doctors.
Regarding those with severe cognitive impairment due to progressive illness, they will not have access to intensive care and will instead be referred to palliative care. For example, a person living with Alzheimer’s could be refused care if their condition has advanced to the point where they are unable to carry out daily and domestic activities independently.
In either of these situations, it is ethically and legally problematic to exclude a person because of their disability. It is imperative that decisions about who will have access to intensive care should be made based on an objective and individualized clinical assessment.
Functional disability assessed using the clinical frailty scale
The second criterion related to functional disability could unfortunately lead to the exclusion of a person with an intellectual disability and a disproportionate number of people living with any form of disability.
Indeed, the measuring instrument to be used for the evaluation, the Clinical Frailty Scale, is unsuitable for people with intellectual disabilities. It is in fact intended for conducting assessments on geriatric clientele.
For example, a patient with Down syndrome incapable of articulating words intelligibly and who has a motor impairment because of his genetic condition will have an excessively high frailty score, which indicates neither poor health nor low probability of survival in and of itself.
The Protocol contains an exclusion criterion that could have a negative impact on people on the ASD: the criterion of functional incapacity, assessed according to the Clinical Frailty Score.
Unfortunately, this criterion could lead to the exclusion of a person with ASD as well as a disproportionate number of people living with any form of disability.
In the same way that the Clinical Frailty Score is not a suitable tool to evaluate people with intellectual disabilities, it is also unsuitable for people who have difficulty performing certain daily activities independently.
A person with ASD would be likely to obtain a high fragility score of 6 or 7, automatically excluding them from access to intensive care, despite this reflecting neither a precarious state of health nor a low probability of survival.
The Protocol contains an exclusion criterion that can have a major impact on people with advanced and irreversible neuromuscular disease.
People with a neuromuscular disorder, such as Parkinson’s or ALS, will unfortunately be denied access to intensive care and will be redirected to palliative care.
It is ethically and legally problematic to exclude a person based solely on their disability. It is imperative that decisions about who will have access to intensive care be made based on an objective and individualized clinical assessment.